Two Diseases, One Response
amfAR argues for a joint response to HIV and HPV, the primary cause of cervical cancer
HIV and cervical cancer, whose primary cause is human papillomavirus (HPV) infection, are intersecting, and often deadly, concerns for women around the world. Addressing these health concerns together, as a new amfAR policy brief suggests, makes sense: The risks for HIV and HPV are bi-directional and mutually reinforcing.
While over 90% of HPV infections are naturally resolved and become undetectable within two years, HIV impairs the body’s ability to spontaneously clear HPV. Women living with HIV (WLHIV) are thus susceptible to chronic, persistent high-risk HPV infection. In fact, WLHIV are six times more likely to develop cervical cancer than those without HIV, and HPV infection doubles the risk of acquiring HIV.
Overlapping HIV Prevalence and Cervical Cancer Incidence per 100,000 Adult Women
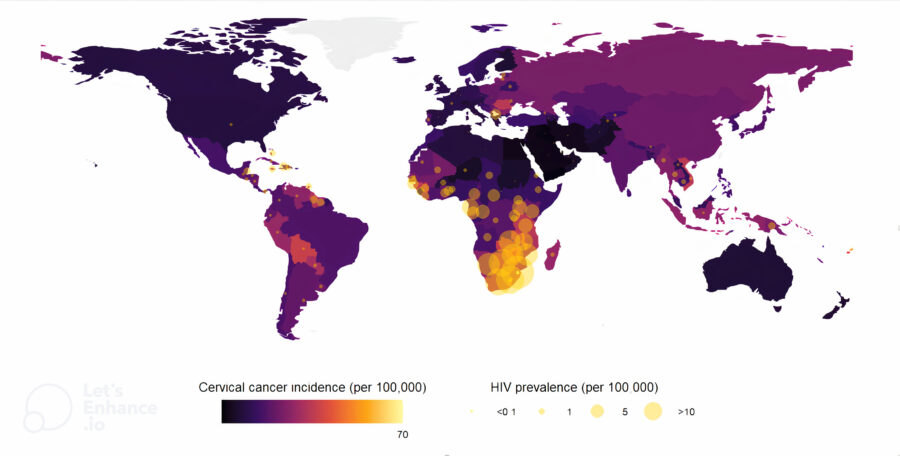
So it’s understandable that countries with the greatest HIV prevalence also rank among the highest for cervical cancer incidence. The highest rates of both diseases are found in sub-Saharan Africa, a region that also has the highest death rates from cervical cancer in the world. were among women
Due to the faster progression of HPV to cervical cancer, WLHIV are an average of 10 years younger at the time of cervical cancer diagnosis than other women.
Despite the urgent need to attend to these health concerns, eff orts to address prevention, treatment, and care for women impacted by these diseases have fallen short.
Early detection of cervical cancer would help avert disease, but current screening rates (HPV testing, primarily) are well below recommended levels for all women, including WLHV.
Not surprisingly, countries with the lowest access to cervical cancer screening also have the highest burden of HIV. In low- and middle-income countries (LMICs), where HIV is most prevalent, only 30% of WLHIV have ever been screened for cervical cancer in their lifetime—compared to 92% in high-income countries.
Cervical cancer is treatable, but many countries suffer from crucial gaps in treatment delivery. For example, the availability of oncologists and chemotherapy in LMICs, such as those in sub-Saharan Africa, is scarce. Over half (55%) of LMICs that offer cervical cancer screening lack radiotherapy and surgery services.
What are the solutions?
One important way to address this dual epidemic is to make sure WLHIV are on sustained antiretroviral therapy, which decreases the risk of cervical cancer by promoting long-term immune health. Another is to increase access to screening tools for both HIV and cervical cancer.

HPV vaccination is also key in preventing cancers, including cervical cancer, and potentially preventing HIV, given the increased risk of HIV acquisition with HPV infection. However, the vaccine is not reaching those most in need. Dr. Annette Sohn, Director of amfAR’s TREAT Asia program in Bangkok, notes that “the few countries in Asia that have begun vaccinating girls against HPV seldom allow adolescents or women to receive the vaccine under their national programs. In addition, people living with HIV require more doses than HIV-negative people.” Strengthening HPV prevention services might be achieved by leveraging infrastructure, and in particular building on HIV service delivery infrastructure often already in place in many high HIV burden countries.
Integration of HIV, HPV, and cervical cancer services is essential. Integrative approaches— training existing HIV clinic staff to address cervical cancer, engaging broad referral networks, and building multi-sectoral partnerships across the public health landscape, among other approaches—would sidestep the limits of previous siloed efforts and make the most of scarce funding. Along with improved health outcomes, integration would reduce the number of return clinic visits, easing the burden of travel, save time and money for service users, and have overall economic benefits for country health systems.
“We are at a critical time in history where we have the tools to both eradicate HIV and cervical cancer as public health threats,” says Dr. Jennifer Sherwood, amfAR’s Director of Research, Public Policy, and one of the lead authors of the brief along with Siena Senn, MPH, former Allan Rosenfield Public Policy Fellow at amfAR. “National governments, donors, policymakers, and researchers can prioritize these overlapping issues through policy, integrated programming, and increased collaborative investment strategies to see the end of both deadly diseases.”
For more information, read amfAR’s policy brief, Dual Epidemics: Leveraging HIV Infrastructure to Support HPV Prevention here.
Click Here to read more from the December 2024 issue of amfAR INNOVATIONS.
Share This:
